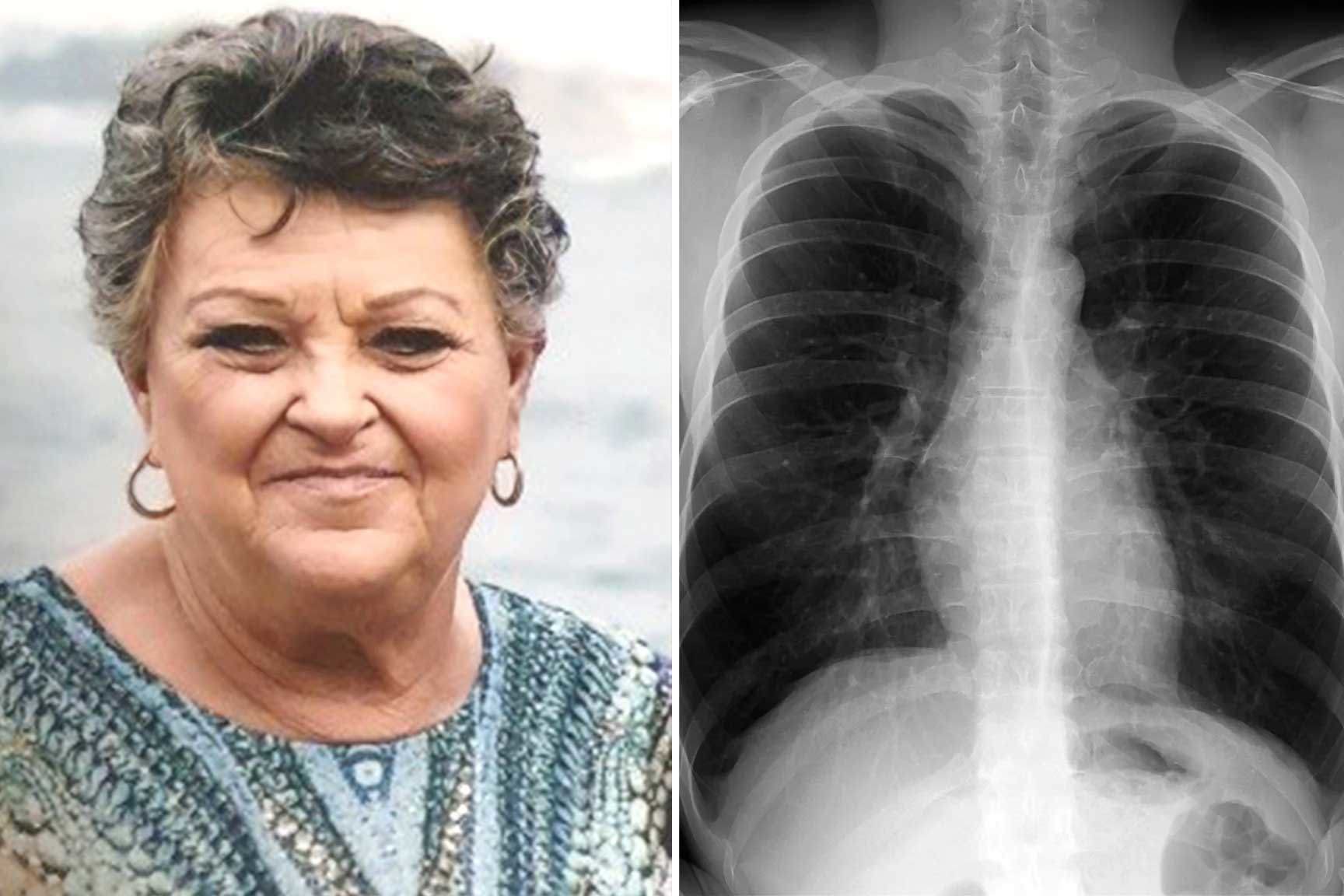
When Sydney woman Linda Goldsmith started having trouble breathing about 15 years ago, she put it down to moving house.
“I was getting breathless, and I don’t often get colds, but when I did, they were a lot worse than normal,” she said.
“I recently moved from the Central Coast back to Sydney, so I thought it was probably just the air in the area.”
Goldsmith went to the doctor, who thought she might have asthma.
READ MORE: The top-paying, low-stress jobs with good salaries in Australia
“I was told I had asthma. I was taking Ventolin, and in winter, the doctor gave me a preventer thing to take as well,” she said.
It wasn’t until about five years later that Goldsmith discovered the true cause of her breathlessness when she ended up at Westmead Hospital with a bad lung infection.
Goldsmith was diagnosed with Chronic Obstructive Pulmonary Disease (COPD), an incurable lung condition that interferes with airflow into the lungs, making it hard to breathe.
Each year, more than 7600 Australians lose their lives to COPD and 53,000 people aged 45 are hospitalised with the condition.
COPD is remarkably common, affecting one in 13 Australians over the age of 40 – but only half know they have it.
Today, the first clinical care standard for COPD has been released by the Australian Commission on Safety and Quality in Health Care in a bid to tackle the low rates of diagnosis and help keep patients with the disease well.
The guidelines have been endorsed by 20 peak bodies, including the Thoracic Society of Australia and New Zealand and Lung Foundation Australia.
Dr Lee Fong, a GP and medical advisor for the commission, said one of the reasons why COPD often took so long to get diagnosed was because of its slow progression.
“COPD is a condition that kind of creeps up on you,” he said, adding that sometimes patients didn’t think to mention gradually worsening coughs or shortness of breath with their GP.
The lung disease also had a lot of symptoms in common with other conditions like asthma, such as shortness of breath, a chronic cough, mucus and wheezing, which could lead to confusion, Fong said.
“That really highlights the importance of getting the diagnosis right, if you don’t have the right diagnosis, you don’t get the best treatment,” he said.
Anyone who often felt short of breath, was wheezing or had persistent “wet” cough, they should talk to their doctor and get tested for COPD.
The only way to diagnose COPD is through a breathing test called spirometry.
The new guidelines outline the correct treatment for COPD which includes a patient action plan and may also involve inhaler medicines and pulmonary rehabilitation.
After her diagnosis, Goldsmith said she received an incredible amount of support to manage her symptoms and reduce flare-ups from clinicians and specialists at Westmead Hospital, where she has completed pulmonary rehabilitation programs and attends a breathlessness clinic.
“When you have COPD, you need to know when you’ve got a trigger, and it doesn’t have to be a cold, it can be changing the weather, or you can get a COPD flare-up for absolutely no reason,” she said.
“It’s important that you know that you’ve got it and get an action plan.”
Do you have a story? Contact reporter Emily McPherson at emcpherson@nine.com.au
links to content on ABC
9News





